Semaglutide and Tirzepatide for PCOS: Evidence-Based Benefits for Hormones, Insulin Resistance, and Weight
- Joshua Silva, MD
- Nov 23, 2025
- 6 min read
Updated: Dec 19, 2025
Polycystic Ovary Syndrome (PCOS) is a complex condition—one that affects millions of women and involves far more than the ovaries. Up to 10–15% of women of reproductive age meet diagnostic criteria, and as many as 65–95% experience insulin resistance, even when they are not overweight.
Because PCOS is both a hormonal and metabolic disorder, treatments that improve insulin sensitivity—like semaglutide (GLP-1) and tirzepatide (GLP-1/GIP)—are emerging as powerful options for improving symptoms, metabolic health, and fertility outcomes.
This article breaks down what the research shows these medications can and cannot do, and how they may help individuals with PCOS.
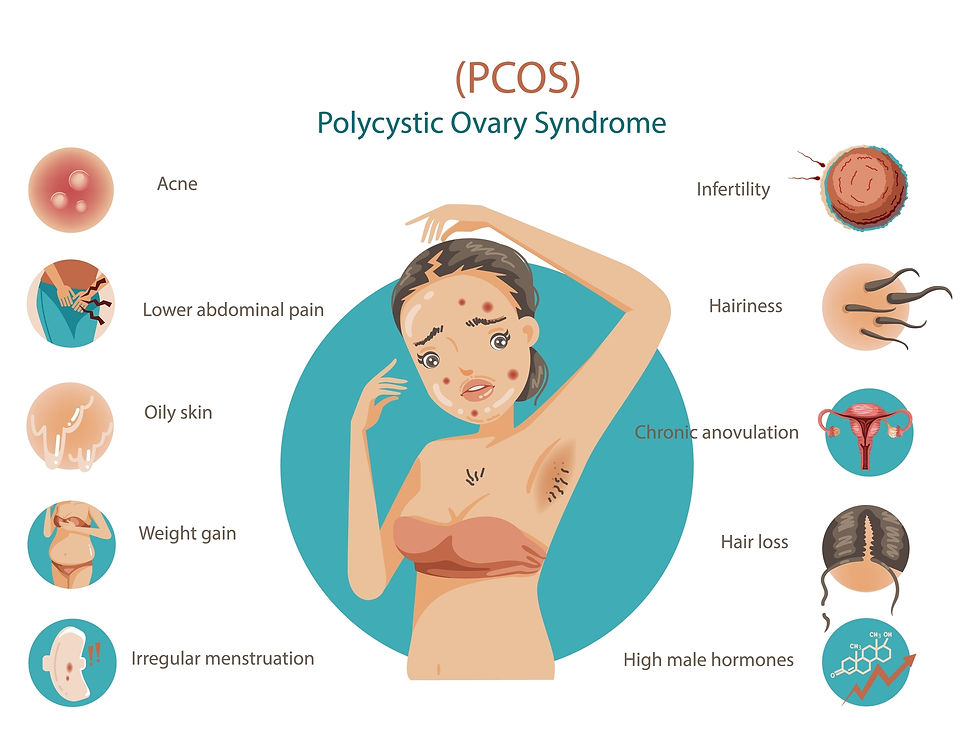
What Is PCOS? Understanding Symptoms, Causes, and Hormonal Imbalances
Polycystic Ovary Syndrome is defined by at least two of the following:
Irregular or absent ovulation
Excess androgens (high testosterone, acne, or excess hair growth)
Polycystic ovarian appearance on ultrasound
But PCOS is not just a reproductive disorder—it is deeply connected to metabolic health.
Insulin resistance is one of the core drivers.
High insulin levels stimulate the ovaries to produce excess testosterone, disrupt normal ovulation, increase hunger and cravings, and contribute to weight gain—creating a self-reinforcing cycle.
This is why many women with PCOS struggle with symptoms such as:
Difficulty losing weight
Irregular cycles
Acne or excess hair growth
Sugar cravings and “crashes”
Fatigue
Infertility
PCOS also increases the long-term risk of:
Prediabetes and type 2 diabetes
Fatty liver disease (MASLD)
High cholesterol
Sleep apnea
Pregnancy complications
Addressing insulin resistance is often the key to improving hormonal symptoms over time.
Do Semaglutide and Tirzepatide Help PCOS? Evidence-Based Benefits
Yes—consistent research shows they can improve both metabolic and hormonal features of PCOS.
Semaglutide and tirzepatide work by activating incretin hormone receptors (GLP-1, and for tirzepatide, both GLP-1 + GIP). These pathways improve insulin sensitivity, reduce blood sugar fluctuations, and help regulate appetite.
Across multiple large studies in PCOS populations, these medications have been shown to:
✔ Improve insulin resistance
Many studies show significant reductions in fasting insulin and improved HOMA-IR (a mathematical calculation used to estimate and quantify insulin resistance) —especially when weight loss is achieved.
✔ Promote meaningful weight loss
This is one of the strongest effects, and weight loss alone can improve PCOS symptoms across the board.
✔ Lower androgen levels
Several trials demonstrate decreases in:
Total testosterone
Free androgen index
DHEA-S
Hirsutism (male distribution hair growth) scores (in some studies)
✔ Improve ovulation and menstrual regularity
While these are not fertility medications, women often experience:
More regular cycles
Improved ovulation markers
Higher natural conception rates in some studies, especially when combined with metformin
✔ Improve metabolic health
GLP-1–based medications improve:
Triglycerides
Cholesterol
Liver fat (MASLD)
Inflammation markers (C-reactive protein)
These improvements reduce long-term risks often associated with PCOS.
Do Semaglutide or Tirzepatide Cure PCOS? What Treatment Research Shows
No. PCOS is not curable—but it is highly treatable.
The medical community has defined PCOS as a chronic but highly modifiable (treatable) condition when underlying factors are addressed.
Unfortunately, semaglutide and tirzepatide do not eliminate the underlying genetic tendencies that make someone prone to PCOS.
However…
They can dramatically reduce the symptoms and metabolic disruptions that make PCOS difficult to manage.
When insulin resistance improves and weight is reduced:
Testosterone levels often decline
Cycles may normalize
Ovulation improves
Fertility can increase
Hunger and cravings stabilize
Energy improves
These changes can make PCOS far easier to live with, even though the condition itself is lifelong.
How Semaglutide and Tirzepatide Work for PCOS: Mechanisms and Hormonal Effects
Here are the mechanisms that matter most for PCOS:
1. Improving Insulin Resistance (the most important effect)
Lowering fasting insulin
Improving glucose control
Reducing post-meal spikes
Lessening compensatory hyperinsulinemia
Since high insulin directly stimulates ovarian androgen production, improving insulin resistance often leads to lower testosterone and improved ovulation.
2. Reducing Androgen Production
By reducing insulin, these medications normalize the hormonal signals sent to the ovaries. This can lead to:
Lower total and free testosterone
Reduced ovarian volume
Less androgen-driven symptoms over time
3. Supporting Healthy, Sustainable Weight Loss
Even modest weight loss (5–10%) can dramatically improve:
Cycle regularity
Fertility markers
Insulin sensitivity
Inflammation
Energy and mood
Semaglutide and tirzepatide routinely achieve far more than 5–10% weight loss when used correctly under medical supervision.
4. Calming Appetite, Cravings, and Blood Sugar Swings
Women with PCOS often experience heightened cravings, reactive hypoglycemia, and difficulty feeling full.
GLP-1 medications smooth these swings and help restore normal hunger signals.
5. Potential Direct Effects on Reproductive Hormones (Emerging Research)
Early studies suggest these medications may also influence:
LH (luteinizing hormone) pulsatility
Hypothalamic reproductive centers
Gonadotropin signaling
While promising, these effects are not fully understood and should be described as emerging, not definitive.
Who Benefits Most From GLP-1 Medications for PCOS?
Not necessarily.
These medications are most effective when PCOS is strongly linked to:
Insulin resistance
Weight gain or difficulty losing weight
Prediabetes or elevated fasting insulin
Androgen excess driven by metabolic dysfunction
Some women primarily have lean-PCOS with minimal metabolic disturbance—this group may experience less improvement from GLP-1–based medications.
A consultation with a physician trained in PCOS + metabolic care is essential to determine if GLP-1 therapy is appropriate.
PCOS and GLP-1 Medications: Frequently Asked Questions
Can I use semaglutide or tirzepatide while trying to conceive?
Generally, no—these medications should be stopped prior to pregnancy. However, optimizing weight, insulin sensitivity, and hormone balance before pregnancy often improves fertility when the time comes.
Will the benefits go away if I stop treatment?
Improvements may continue as long as weight and insulin levels remain stable. Some symptoms can return gradually if weight is regained or insulin resistance worsens.
Is tirzepatide better than semaglutide for PCOS?
Early research suggests tirzepatide may offer greater improvements in weight and insulin resistance, but both are highly effective. The best choice depends on your medical profile.
Do I still need metformin?
Many women benefit from combination therapy (metformin + GLP-1). This should be individualized.
The Bottom Line: Should You Use GLP-1 Medications for PCOS?
Semaglutide and tirzepatide do not cure PCOS, but they are among the most effective tools we have for improving the metabolic and hormonal disturbances that fuel PCOS symptoms.
For many women, addressing insulin resistance leads to:
Lower androgen levels
More regular cycles
Better ovulation
Easier weight control
Improved fertility
Better metabolic health long-term
At Potere Health MD, we provide evidence-based, physician-guided treatment plans that address the root causes of PCOS—not just the symptoms.
If you’re struggling with weight, cravings, irregular cycles, or difficulty losing weight with PCOS, we can help you find the right medical approach for your body.
Disclaimer:
This article is for educational purposes only and is not a substitute for medical advice.
About the Author
Dr. Joshua Silva, MD, is a licensed physician and Medical Director of Potere Health MD. After graduating medical school from the University of Hawaii, he completed residency training in Occupational and Environmental Medicine from the University of Utah where he also earned a master's degree in Occupation Health. He now specializes in evidence-based weight management, including GLP-1/GIP therapies (semaglutide & tirzepatide). Dr. Silva provides in-person and virtual care for patients with clinics in Salt Lake City, St. George, and Cedar City, Utah.
Sources:
1. Elkind‐Hirsch K, Chappell N, Shaler D, et al. Liraglutide 3 mg on weight, body composition, and hormonal and metabolic parameters in women with obesity and PCOS: a randomized placebo-controlled phase 3 study. Fertil Steril.2022;118(2):371-381. doi:10.1016/j.fertnstert.2022.05.012.
2. De Hollanda BAA, de Araújo FM, de Souza ACC, et al. The efficacy and safety of GLP-1 agonists in PCOS women living with obesity: a meta-analysis of randomized controlled trials. J Diabetes Complications. 2024;38(1):108680. doi:10.1016/j.jdiacomp.2024.108680. https://pubmed.ncbi.nlm.nih.gov/39178623/
3. Carmina E, Longo RA. Semaglutide treatment of excessive body weight in obese PCOS patients unresponsive to lifestyle programs. J Clin Med. 2023;12(18):5793. doi:10.3390/jcm12185793.
4. Huang R, He Y. The safety and efficacy of liraglutide combined with metformin in clinical treatment of polycystic ovary syndrome patients: a meta-analysis. BMC Womens Health. 2025;25(1):282. doi:10.1186/s12905-025-03787-z. https://pubmed.ncbi.nlm.nih.gov/40481408/
5. Chen H, Zhang W, Gao Y, et al. Effects of combined metformin and semaglutide therapy on metabolic and reproductive outcomes in PCOS. Reprod Biol Endocrinol. 2025;23(1):54. doi:10.1186/s12958-025-01213-4.
6. Nylander M, Frøssing S, Kistorp C, et al. Liraglutide in polycystic ovary syndrome: a randomized trial investigating effects on thrombogenic potential. Endocr Connect. 2017;6(2):89-99. doi:10.1530/EC-16-0094.
7. Siamashvili M, Davis SN. Update on the effects of GLP-1 receptor agonists for the treatment of polycystic ovary syndrome. Expert Rev Clin Pharmacol. 2021;14(9):1081-1089. doi:10.1080/17512433.2021.1933433.
8. Lin S, Deng Y, Huang J, et al. Efficacy and safety of GLP-1 receptor agonists on weight loss and insulin resistance in polycystic ovary syndrome: a systematic review and meta-analysis. Sci Rep. 2025;15:99622. doi:10.1038/s41598-025-99622-4.https://www.nature.com/articles/s41598-025-99622-4
9. Cassar S, Misso ML, Hopkins WG, et al. Insulin resistance in polycystic ovary syndrome: a systematic review and meta-analysis of euglycaemic–hyperinsulinaemic clamp studies. Hum Reprod. 2016;31(11):2619-2631. doi:10.1093/humrep/dew218.
10. Su P, Qiao S, Han Y, et al. Physiopathology of polycystic ovary syndrome in endocrinology, metabolism and inflammation. J Ovarian Res. 2025;18(1):34. doi:10.1186/s13048-025-01621-6.




Comments